I read with great astonishment the newly published article in this month issue of SOARD titled “An investigation of the neural mechanisms underlying the efficacy of the adjustable gastric band”. The authors attempt to find an alternative mechanism of action besides mechanical restriction for the Lap Band. They rightly admit that restriction by itself does not lead to durable weight loss. Neuro-hormonal changes are the underlying mechanism for weight loss after gastric bypass and gastric sleeve surgery. Indeed, changes in Ghrelin, GLP-1 and PYY are the hallmark for successful metabolic procedures. However, no such changes have ever been demonstrated with adjustable gastric banding. This is most likely why Lap Band, as a weight loss procedure, has failed. Consequently, Lap Band has been reduced to a purely restrictive procedure, and rightly so, with poor long-term weight loss results. The assumption that filling the band with saline in order to “ optimize” restriction to controls hunger and promote weight loss has failed the test of time. This absurd assumption remains a painful reminder of how ignorant we were and how deficient our knowledge about obesity was just few years ago. Thousands of Lap Band patients have failed to loose weight. Many suffered from band related complications like erosion, slippage, esophageal dysmotility and dilation, acid reflux, aspiration pneumonia… in hopeless attempts to beat obesity and regain their healthy lives. This large-scale human trial, however, is still not enough for some Lap Band proponents and the company that manufactures Lap Bands.
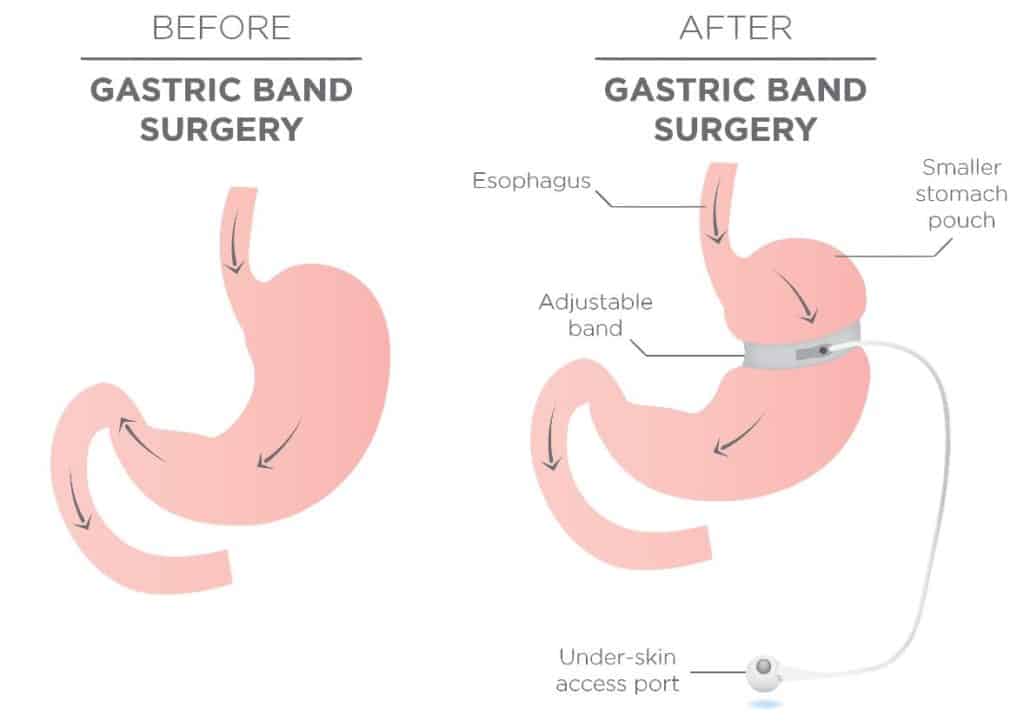
In a rather desperate attempt, the authors of this article devise an elaborate weight loss trial in a rodent model. The authors assume that stretch receptors in the small gastric pouch above the inflated Lap Band are activated and send neural signals via the vagus nerve to the brainstem to promote satiety and weight loss. By denervating the afferent vagal nerve fibers using capsaicin, in a rat model, the authors showed abolished Lap Band induced weight loss.
I am a huge proponent of studying mechanisms of action of bariatric surgery. The neural component of metabolic surgery is still a black box. The gastro-intestinal system communicates with the central nervous system in a variety of ways. The vagus nerve is logically one of these communication pathways relaying thousands from the gut to the brain. However, we don’t understand these signals. Therefore, we don’t know how to manipulate these signals to promote weight loss and satiety. Assuming that stretch receptors in the gastric pouch above the inflated band, control satiety is quite naïve. I should mention that the pouch created by the band is not gastric in nature but rather esophageal. The only sure consequence of esophageal constriction is esophageal dysmotility and dilation.
One interesting observation we have learned from the large-scale, worldwide, lap Band human trial is that a minority of band patients does lose weight and maintain it for the long run. Those lucky patients require very little band adjustment. One or two band fills at most. They report increased satiety, small meal consumption without any nausea, vomiting, heartburn or discomfort. These patients are definitely worth studying, in my opinion, to figure out Lap Band mechanism of action. Do these patients have a decrease in fasting Ghrelin? Is their postprandial GLP-1 higher? Is their gastric fundus smaller in size than what we typically see in overweight patients? Is the gastric fundus excessively imbricated over the band?
Going back to a rodent model with all its deficiencies to demonstrate a failed weight loss concept doesn’t make lot of sense to me.