The patient is a 51-year-old female who underwent a gastric sleeve in 2006 at one of the hospitals in the medical center in Houston. She lost around 30 pounds during the first year after surgery and maintained around 25 pound weight loss over the past 10 years. The patient reports that prior to surgery she experienced heartburn at least twice weekly and food regurgitation from time to time. Prior to surgery she was not evaluated for acid reflux disease by endoscopy, barium swallow or pH Bravo capsule. During surgery, her hiatal hernia that may have been smaller at the time was not investigated. The operative report mentions that of a 36 French bougie was used to perform the gastric sleeve.
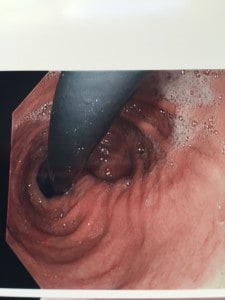 Shortly after surgery and for the past 10 years the patient has been struggling with severe acid reflux related symptoms including heartburn and food regurgitation. She reports nighttime symptoms that prevent her from sleeping with fatigue and somnolence during the day. As usual the patient was placed on escalating doses of PPIs in hopeless attempts to control her symptoms. Following presentation to my office, she underwent an upper endoscopy that showed a sliding hiatal hernia and laxity in the hiatal opening. The distal esophagus was inflamed despite high dose PPI. The gastric fundus was incompletely resected and there was no narrowing at the incisura. An UGI showed obvious contrast reflux into the esophagus, and a large gastric fundus where contrast pooled and slowly passed into the distal stomach.
Shortly after surgery and for the past 10 years the patient has been struggling with severe acid reflux related symptoms including heartburn and food regurgitation. She reports nighttime symptoms that prevent her from sleeping with fatigue and somnolence during the day. As usual the patient was placed on escalating doses of PPIs in hopeless attempts to control her symptoms. Following presentation to my office, she underwent an upper endoscopy that showed a sliding hiatal hernia and laxity in the hiatal opening. The distal esophagus was inflamed despite high dose PPI. The gastric fundus was incompletely resected and there was no narrowing at the incisura. An UGI showed obvious contrast reflux into the esophagus, and a large gastric fundus where contrast pooled and slowly passed into the distal stomach.
It became readily apparent that the patient had an incompletely resected gastric sleeve that lead to poor weight loss and acid reflux. The problem is anatomic and the treatment is surgery rather than high dose PPIs. Indeed, a well-performed gastric sleeve surgery effectively eliminates acid reflux. However, an incomplete gastric sleeve resection is a sure recipe for acid reflux disease or GERD. Narrowing or twisting the gastric sleeve tube at the level of the incisura also results in acid reflux. A hiatal hernia further contributes to the reflux pathophysiology.
 I have encountered several cases so far in my career of sleeve induced acid reflux. Invariably, a retained gastric fundus was present. Mechanical or functional narrowing of the incisura does contribute to acid reflux and food regurgitation. However, in this particular case the incisura was widely open on endoscopy and UGI. The gastric fundus seemed to be the main culprit especially with a widely open hiatus. A retained gastric fundus may contribute to intermittent relaxation of the lower esophageal sphincter leading to reflux. Furthermore the gastric fundus may allow for an acid pocket to form in the vicinity of the gastric cardia leading to acid reflux. A retained gastric fundus may also cause delayed gastric emptying further exacerbating acid reflux. The gastric fundus is a posterior structure and it can easily be incompletely resected during sleeve surgery. When properly resected, acid reflux resolves. Fixing the hiatal hernia alone is not enough. A wide hiatal opening and the presence of a sliding hernia are two factors that contribute to acid reflux. They are not however the only or most important factors. In this particular case, I performed a hiatal hernia repair with gastric fundus resection. Patient was very satisfied after surgery with complete resolution of her acid reflux related symptoms. She also lost 46 more pounds in 6 months. Other cases with narrowing of the incisura were converted to gastric bypass with excellent acid reflux resolution. LINX procedure for acid reflux cases after sleeve surgery has been reported. It is obvious that in this particular case LINX surgery is completely useless. In general, I don’t think that LINX surgery has any role in treating any form of acid reflux disease. Hopefully, future studies will demonstrate my point of view.
I have encountered several cases so far in my career of sleeve induced acid reflux. Invariably, a retained gastric fundus was present. Mechanical or functional narrowing of the incisura does contribute to acid reflux and food regurgitation. However, in this particular case the incisura was widely open on endoscopy and UGI. The gastric fundus seemed to be the main culprit especially with a widely open hiatus. A retained gastric fundus may contribute to intermittent relaxation of the lower esophageal sphincter leading to reflux. Furthermore the gastric fundus may allow for an acid pocket to form in the vicinity of the gastric cardia leading to acid reflux. A retained gastric fundus may also cause delayed gastric emptying further exacerbating acid reflux. The gastric fundus is a posterior structure and it can easily be incompletely resected during sleeve surgery. When properly resected, acid reflux resolves. Fixing the hiatal hernia alone is not enough. A wide hiatal opening and the presence of a sliding hernia are two factors that contribute to acid reflux. They are not however the only or most important factors. In this particular case, I performed a hiatal hernia repair with gastric fundus resection. Patient was very satisfied after surgery with complete resolution of her acid reflux related symptoms. She also lost 46 more pounds in 6 months. Other cases with narrowing of the incisura were converted to gastric bypass with excellent acid reflux resolution. LINX procedure for acid reflux cases after sleeve surgery has been reported. It is obvious that in this particular case LINX surgery is completely useless. In general, I don’t think that LINX surgery has any role in treating any form of acid reflux disease. Hopefully, future studies will demonstrate my point of view.

