Last week I published a blog about acid reflux developing after gastric sleeve surgery in the setting of a hiatal hernia. Subsequently, I have received several questions from a number of followers and readers about acid reflux developing after Lap Band conversion to sleeve surgery. This is a very important topic especially that these days we are experiencing a high rate of band removal and conversion to other weight loss procedure for either worsening acid reflux related symptoms or failure to lose weight.
Lap band conversion to gastric sleeve surgery is a tricky surgery and ought to be approached with extra care in order to avoid unnecessary complications. Most of the questions I have received were related to worsening acid reflux following lap band conversion to sleeve. In particular, does a retained gastric fundus cause acid reflux following band conversion to sleeve. The short answer is yes. There are many reasons for GERD to worsen or develop de novo when converting a band procedure to gastric sleeve. Let’s explore them one by one.
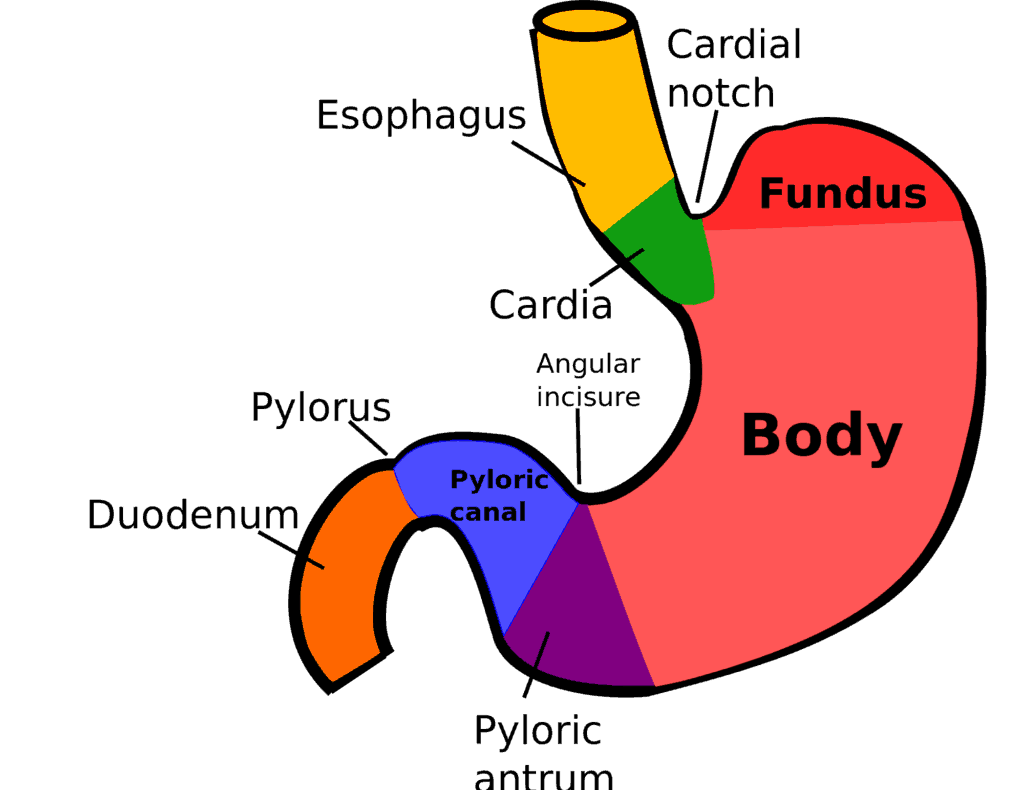
First, almost all lap band patients have some degree of esophageal dysmotility secondary to years of band restriction or over-restriction. It is not normal to impede the free flow of food from the esophagus into the stomach. Placing a barrier in this high compliance, low resistance area forces the esophagus to work harder to transfer food into the stomach. The end result is a wide spectrum of esophageal dysmotility patterns ranging from low wave contractile amplitude to a full blown pseudo-achalasia condition. The esophagus, cardia and hiatal opening dilate in response to long-term band restriction. A hiatal hernia may develop and tertiary esophageal contractions are almost invariably noted on contrast studies. All these physiologic changes contribute to acid reflux disease. Adding a poorly constructed gastric sleeve (large retained gastric fundus, twisted sleeve lumen and/or narrowing at the incisura angularis) further exacerbates the underlying acid reflux problem. Particularly relevant to lap band conversion to gastric sleeve is the incompletely resected gastric fundus. Due to thick fibrotic tissue developing around the upper gastric fundus, a proper gastric fundus mobilization and resection may sometimes be difficult if not impossible. I personally stage all my lap band conversion to gastric sleeve for two reasons. First, almost all studies on this subject have demonstrated a lower leak rate by staging the conversion. Second, by allowing the scar tissue to remodel following band removal, gastric fundus dissection and resection is more adequate. Part of the gastric fundus is contracted and has retracted due to scar tissue development. Leaving part of the gastric fundus un-resected in the setting of a dilated hiatus and poor esophageal function and super-imposing the high pressure system associated with gastric sleeve surgery is a recipe for GERD.
For all these reasons, converting a lap band to gastric sleeve should only be done after careful consideration. My approach is as follows:
- I decompress the band from all fluid content
- I perform a baseline UGI to check for esophageal dilation, tertiary contractions, hiatal hernia
- I perform an esophageal manometry for any patient suffering from persistent dysphagia or GERD related symptoms after band decompression
- I repeat the UGI in 8 weeks and document resolution of esophageal dilation
- Any patient with persistent esophageal dilation undergoes an esophageal manometry to assess esophageal motility
- Lap band conversion to sleeve is offered only if esophageal motility is within normal
- Lap band conversion to sleeve is staged and hiatal hernia repair is added if needed
- Patients with persistent esophageal dilation, dysmotility, or GERD related symptoms are offered lap band conversion to gastric bypass. I have had great success in GERD related symptom improvement with gastric bypass. The Roux limb creates a negative pressure system that promotes esophageal emptying and prevents food regurgitation and reflux.
Patients who have undergone lap band conversion to gastric sleeve and are experiencing acid reflux symptoms ought to be thoroughly re-evaluated. Gastric sleeve surgery can be easily revised into gastric bypass with very high success rate and minimal morbidity and mortality in properly selected cases. If you are a bariatric patient and suffers from heartburn, food regurgitation, nighttime cough or difficulty swallowing give us a call. We offer comprehensive acid reflux testing in a center of excellence for obesity and acid reflux management.